|
Case Report
Medullary ischemia: Clinical and radiological approach
1 Medical Imaging Department, National University Hospital Center of Fann, Dakar, Senegal
2 Neurology Department, National University Hospital Center of Fann, Dakar, Senegal
3 Medical Imaging Department, Principal Hospital of Dakar, Dakar, Senegal
Address correspondence to:
Mbaye THIAM
Medical Imaging Department, National University Hospital Center of Fann, Dakar,
Senegal
Message to Corresponding Author
Article ID: 100018R02MT2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
THIAM M, MBAYE KA, DIAGNE R, FALL A, DIOUF KN, BA S. Medullary ischemia: Clinical and radiological approach. Edorium J Radiol 2021;7:100018R02MT2021.ABSTRACT
Introduction: Spinal cord infarction is a serious neurovascular emergency due to its short-, medium-, and long-term complications.
Case Report: A 54-year-old patient with no previous history or particular condition hospitalized for an acute spinal cord injury, with magnetic resonance imaging (MRI) showing medullar ischemia without any etiology found. The evolution was marked by a good motor evolution.
Conclusion: Medullary infarction is a serious pathology under-diagnosed in our context because of the difficult accessibility of MRI.
Keywords: Ischemia, MRI, Spinal cord
INTRODUCTION
Medullary infarction is a serious neurovascular emergency due to its short-, medium-, and long-term complications. Spinal cord ischemia is under-diagnosed in our continent due to the difficult accessibility of magnetic resonance imaging (MRI), which is the examination of choice for the diagnosis of spinal cord vascular damage, and also due to its clinical similarities with acute spinal cord injury (inflammatory damage, vascular malformation, spinal bleeding). The etiologies are numerous and heterogeneous such as traumatic causes, arterial dissection, hypotension, atherosclerosis, toxicity, fibrocartilage embolization, sub-renal abdominal aneurysm repair, epidural anesthesia, and vasculitis [1],[2]. We describe the clinico-radiological aspects of a 54-year-old female patient diagnosed with spinal cord ischemia.
CASE REPORT
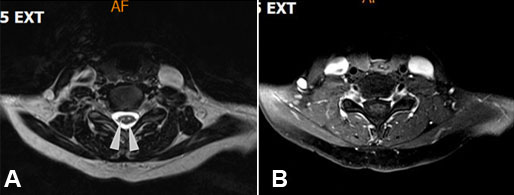
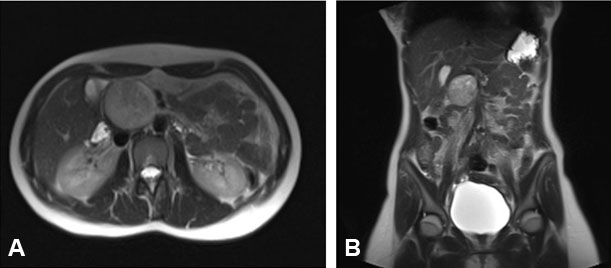
A 54-year-old female patient with no previous history or particular condition was seen for a motor deficit of the four limbs of sudden onset, preceded by a few minutes of painful cramps, first cervical and then rapidly diffuse, affecting the whole body. A few hours after the deficit, she presented genital-sphincter disorders such as acute urine retention and constipation. There were no visual or respiratory disorders. The clinical examination showed a clear consciousness, a syndrome of medullary interruption made of neurovegetative disorder and bilateral pyramidal syndrome without sensory level. Spinal cord MRI was performed three weeks later with sequences sagittal T1 and T2 STIR, axial T1 and T2, and axial and sagittal T1-weighted after gadolinium. It showed an intramedullary T2 STIR linear high signal intensity named pencil like sign extending from C5 to D2 (Figure 1), low signal intensity in T1 not enhanced after injection (Figure 2B). Axial T2-weighted image shows bilateral and symmetric ovoid foci hyperintensities in the ventral cord also known as the owl eyes sign (Figure 2A). Within the framework of the etiological research, the biological assessment was without particularity with lipidic assessment and normal blood count, fasting glycemia at 0.87 g/L and normal syphilitic and retroviral serologies. Cardiac exploration [transthoracic and transesophageal cardiac echography, electrocardiogram (ECG) and ECG Holter] to search for emboligenic heart disease and atheromatous plaques at the level of the aortic arch was normal. The exploration of the supra-aortic trunks did not show any particular abnormality. After a symptomatic treatment, a progressive recovery was noted in our patient with a muscular strength of 4/5, but on the sensory level we noted a persistence of cramps.
DISCUSSION
Medullary ischemia is a rare pathology. Unlike ischemic stroke there are no epidemiological data evaluating the prevalence and incidence of spinal cord ischemia [3]. It most often affects elderly subjects with a male predominance [3] without any valid explanation. The clinical picture is most often suggestive without any particular specificity, making it difficult to differentiate from other causes of acute transverse myelitis [4]. Ischemia of the anterior spinal artery (ASA) is more frequent than ischemia of the posterior spinal artery (PSA). This is explained by the differences in the number and distribution of radiculomedullary arteries destined to the anterior and posterior systems. The clinical manifestations depend on the affected arterial territory. In ischemia of the ASA, the infarction may involve the entire arterial territory, most often bilaterally, or be limited to the central territory of this artery, which may be affected in whole or in part. In our patient, the ischemia involved the ASA and the clinical manifestations are similar to those described in the literature [3],[5]. In the infarction of the entire ASA, the clinical manifestations are not purely motor, there may be neurovegetative manifestations (sphincter disorders) or sensory and the latter is explained by the damage of the sensory fibers that decrescendo (thermoalgesic) and the fact that the anterior spinal artery vascularizes the deep part of the posterior cords and the posterolateral part of the lateral cord. Classically, the neurological deficit is preceded by acute spinal and/or radicular pain [5]. Spinal cord infarcts are most often found in the lumbar or cervical bulge and respiratory signs are seen in upper cervical involvement. Infarcts in the territory of Adamkiewicz’s artery result in paraplegia and sometimes early amyotrophy of the lower limbs reflecting extensive involvement of the anterior horns in height [5]. Medullary MRI is an important element in the diagnosis of spinal cord infarction. It must be performed in the axial (to identify the arterial territory involved) and sagittal (to determine the extent of the lesion in height) planes with gadolinium injection. Several aspects are described according to the evolution of the clinical picture. Before the 12th hour, imaging may be normal and allows to eliminate other causes of acute spinal cord injury, such as intraspinal hematoma. Signs are often not specific for spinal cord infarction. After the 12th hour or more often the 24th hour, the infarction is reflected by a T2 high signal intensity and a T1 isosignal or low signal intensity, within an edematous marrow. Contrast enhancement reflecting a rupture of the blood-medullary barrier may be observed after one to three weeks and spinal cord atrophy in chronic forms. Infarcts involving the entire anterior spinal arterial territory show a hypersignal in the anterior two-thirds of the medulla, but often the lesion predominates in the central territory where it may be relatively limited to the gray matter, giving the so-called “owl’s eyes” appearance [6]. In these central infarcts, the high signal intensity may spill over into the adjacent white matter or involve only the gray matter of the anterior horns, resulting in the “snake eyes” appearance [3],[6]. Infarcts in the posterior spinal territory show high signal intensity of the posterior cords and the adjacent part of the lateral cords. In the late stage, the infarction appears as a cavity image [7]. Diffusion-weighted imaging (DWI) is diagnostic in the acute phase of spinal cord infarction by showing an unspecific high signal intensity (DWI high signal intensity in 62% of myelitis) and a lowered apparent diffusion coefficient [8], but the quality of diffusion-weighted echo-planar images is reduced because of sensitivity artifacts due to the heterogeneous magnetic environment of the spine, which can create false-positive results.
The etiologies are numerous and heterogeneous; a rigorous and contextualized approach remains necessary in our context. The evolution is most often unfavorable [5],[6] and depends on the topography of the lesion. While upper cervical lesions are more often life-threatening in the short term, dorsal and lumbar lesions have a greater impact on the functional level with long-term complications of decubitus. In our patient we noted a good evolution.
CONCLUSION
Medullary ischemia is a serious pathology that is under-diagnosed in our context because of the difficult accessibility of MRI and the similarities with other causes of acute spinal cord injury. A good diagnostic approach is more than necessary for an optimal management.
REFERENCES
1.
Hong DK, Lawrence HM. Anterior spinal artery syndrome following total hip arthroplasty under epidural anaesthesia. Anaesth Intensive Care 2001;29(1):62–6. [CrossRef]
[Pubmed]

2.
O’Farrell R, Thornton J, Brennan P, Brett F, Cunningham AJ. Spinal cord infarction and tetraplegia—rare complications of meningococcal meningitis. Br J Anaesth 2000;84(4):514–7. [CrossRef]
[Pubmed]

3.
Weidauer S, Nichtweiss M, Lanfermann H, Zanella FE. Spinal cord infarction: MR imaging and clinical features in 16 cases. Neuroradiology 2002;44(10):851–7. [CrossRef]
[Pubmed]

4.
Fortuna A, Ferrante L, Acqui M, Trillò G. Spinal cord ischemia diagnosed by MRI. Case report and review of the literature. J Neuroradiol 1995;22(2):115–22.
[Pubmed]

5.
Masson C, Leys D, Meder JF, Dousset V, Pruvo JP. Spinal cord ischemia. [Article in French]. J Neuroradiol 2004;31(1):35–46. [CrossRef]
[Pubmed]

6.
Novy J, Carruzzo A, Maeder P, Bogousslavsky J. Spinal cord ischemia: Clinical and imaging patterns, pathogenesis, and outcomes in 27 patients. Arch Neurol 2006;63(8):1113–20. [CrossRef]
[Pubmed]

7.
Kume A, Yoneyama S, Takahashi A, Watanabe H. MRI of anterior spinal artery syndrome. J Neurol Neurosurg Psychiatry 1992;55(9):838–40. [CrossRef]
[Pubmed]

8.
Loher TJ, Bassetti CL, Lövblad KO, et al. Diffusion-weighted MRI in acute spinal cord ischaemia. Neuroradiology 2003;45(8):557–61. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Mbaye THIAM - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Khalifa Ababacar MBAYE - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rokhaya DIAGNE - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Amath FALL - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Khadiatou Ndiaye DIOUF - Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sokhna BA - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Mbaye THIAM et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.