|
Case Report
Cystic neuro-endocrine tumor of pancreas in 14 years old child: A case report and review of literature
1 MD, Radiology Resident, Radiology Department of Cheikh Zaid Hospital, Rabat, Morocco
2 Resident of Radiology, Cheikh Zaid Hospital, Abulcasis University, Rabat, Morocco
3 Head of Service of Pediatric and Women’s Imaging, CHU Avicenne, Rabat, Morocco
Address correspondence to:
Dounia Najioullah
MD, Radiology Resident, Radiology Department of Cheikh Zaid Hospital, Rabat,
Morocco
Message to Corresponding Author
Article ID: 100017R02DN2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Najioullah D, Laachir G, Chat L. Cystic neuroendocrine tumor of pancreas in 14 years old child: A case report and review of literature. Edorium J Radiol 2021;7:100017R02DN2021.ABSTRACT
Introduction: Neuro-endocrine tumors of the pancreas are rare in children. They are even rarer in their cystic forms and lead to confusion with other pancreatic cysts, especially when it is not functional.
Case Report: We report the case of a 14-year-old girl, in whom radiological exploration for epigastralgia revealed a cyst of the head of the pancreas without repercussions on bile ducts, and which after surgery turned out to be a neuro-endocrine cystic tumor.
Conclusion: Although rare, neuro-endocrine tumor should be mentioned among the diagnoses of cystic mass of the pancreas in children.
Keywords: Child, Cystic, Neuro-endocrine tumor, Pancreas
INTRODUCTION
Neuro-endocrine tumors are uncommon neoplasms which often present diagnostic challenges to both the radiologist and pathologist.
The clinical evaluation of these pancreatic rare tumors is still suffering from same limitations despite the improvement in the diagnostic tools. Subsequently, the aim of this article is to highlight diagnostic pitfalls and differential diagnosis of these tumors particularly in their cystic form.
CASE REPORT
A 14-year-old girl was referred by her pediatrician for possible management of a pancreatic cyst discovered on an abdominal ultrasonography. Our patient suffered from abdominal paroxystic pain accompanied by vomiting.
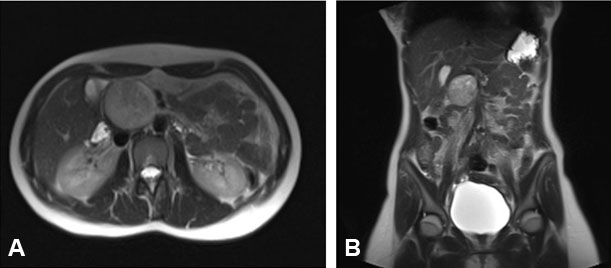
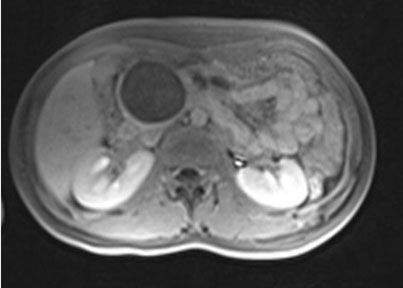
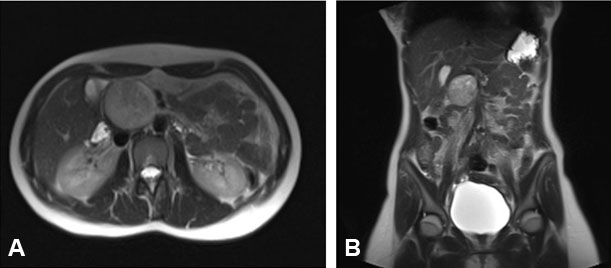
The child was in good general condition. Clinical examination reveals a firm, painless, epigastric mass. The rest of the exam was strictly normal. Ultrasound and abdominal magnetic resonance imaging performed (Figure 1A and Figure 1B) specified a cystic avascular encapsulated lesion of head of pancreas, measuring 48 mm from the long axis oblique out, 45 mm high, 47 mm thick (Figure 2). The pancreatic head was distorted by the cyst pushing the mesenteric vessels toward the periphery, without peritoneal fluid reaction, no perilesional lymph nodes and no communication with the visualized biliary duct.
She underwent exploration laparotomy, which revealed a large cystic swelling with a thick wall. The cyst was dissected and completely removed. Postoperatively, she did well and was discharged home on the eighth postoperative day (Figure 3).
The excised tumor was round, cystic, and well-demarcated with no parietal calcifications.
Histologically, the tumor was composed of sheets of monomorphic medium-sized cells arranged in acinar or glandular pattern, surrounding a lumen, with no visible mitoses or amyloid depositions.
The neuroendocrine differentiation of the tumor is confirmed by the expression of chromogranin and synaptophysin.
DISCUSSION
Pancreatic cysts are extremely rare in the pediatric age population. Pancreatic pseudocysts following acute pancreatitis, whether post-traumatic or post-inflammatory, are the most frequent. True cysts are extremely rare and classified into six types: congenital, retention, duplication, pseudocysts, neoplastic, and parasitic cysts.
Differentiating clinically and radiologically between these types is very difficult. Pathologically, the first three types, called true cyst are true developmental cysts and are circumscribed by true epithelium unlike the pseudo-pancreatic cysts [1],[2],[3],[4].
Gastro-enteropancreatic neuroendocrine tumors (GEP-NETs) are neural crest tumors whose clinical and imaging features are not well described in children population. These tumors arise from neuro-endocrine cells issued from pancreas, gut, and bronchial tree. The term “neuroendocrine tumors” regroup carcinoid tumors, islet cell tumors, and amine precursor uptake and decarboxylation (APUD) tumors [5].
Neuro-endocrine tumors can be subdivided into malignant and benign entities. They represent 20% of malignant pancreatic tumors in children. They may be associated to multiple endocrine neoplasia type 1, most of which are nonfunctioning. They also may be associated to von Hippel–Lindau syndrome though cystic neoplasms are the most commonly seen pancreatic manifestation of this syndrome [5].
Neuro-endocrine tumors account for only 1–2% of all pancreatic neoplasms and less than 10% of all neuroendocrine tumors are cystic, which makes cystic neuro-endocrine lesions very rare.
The clinical presentation of islet cell neoplasms differs between functional and nonfunctional tumors. Nonfunctional tumors present with nonspecific symptoms related to mass effect. Functional tumors, by contrast, often present earlier with symptoms related to the hyper-secreting hormone [5].
Identification of cystic neuro-endocrine tumors in the pancreas with computed tomography (CT) scan or magnetic resonance imaging (MRI) is extremely difficult [6].
These tumors appear as nonspecific circumscribed hypo-echoic pancreatic masses at ultrasound.
The most frequent imaging feature of neuro-endocrine tumors at contrast-enhanced CT and at MRI is hyper-vascularity. They have a greater degree of enhancement than normal pancreas in both the arterial and venous phases of imaging. Some of neuro-endocrine tumors may be cystic; not communicating with bile ducts, the presence of a hypervascular rim suggests this tumor over cystic pancreatic lesions. General MRI signal-intensity characteristics include T1 hypo-intensity and T2 hyper-intensity relative to the normal pancreatic parenchyma.
Modern imaging techniques usually show a well-defined unilocular cyst; however, even with the combined use of laboratory data, clinical features, and diagnostic imaging, it may be difficult to accurately differentiate congenital pancreatic cyst from other nearby cystic lesions of the abdomen. This is especially true if they are large [6].
Endoscopic ultrasound coupled with fine-needle aspiration has enabled not only the detailed examination of pancreatic cystic lesions but also cytological, biochemical, and immune-cytological analysis [7],[8].
The treatment of neuroendocrine cyst is surgical. The type of surgical treatment depends on the site and size of the cyst. Total excision is the treatment of choice [9],[10].
CONCLUSION
Although rare, neuro-endocrine tumor should be mentioned among the diagnoses of cystic mass of the pancreas in children.
REFERENCES
1.
Shet NS, Cole BL, Iyer RS. Imaging of pediatric pancreatic neoplasms with radiologic-histopathologic correlation. AJR Am J Roentgenol 2014;202(6):1337–48. [CrossRef]
[Pubmed]

2.
Al-Salem AH, Matta H. Congenital pancreatic cyst: Diagnosis and management. J Pediatr Gastroenterol Nutr 2014;59(4):e38–40. [CrossRef]
[Pubmed]

3.
Basturk O, Coban I, Adsay NV. Pancreatic cysts: Pathologic classification, differential diagnosis, and clinical implications. Arch Pathol Lab Med 2009;133(3):423–38. [CrossRef]
[Pubmed]

4.
Boulanger SC, Borowitz DS, Fisher JF, Brisseau GF. Congenital pancreatic cysts in children. J Pediatr Surg 2003;38(7):1080–2. [CrossRef]
[Pubmed]

5.
Khanna G, O’Dorisio SM, Menda Y, Kirby P, Kao S, Sato Y. Gastroenteropancreatic neuroendocrine tumors in children and young adults. Pediatr Radiol 2008;38(3):251–359. [CrossRef]
[Pubmed]

6.
Shet NS, Cole BL, Iyer RS. Imaging of pediatric pancreatic neoplasms with radiologic-histopathologic correlation. AJR Am J Roentgenol 2014;202(6):1337–48. [CrossRef]
[Pubmed]

7.
Thorlacius H, Kalaitzakis E, Johansson GW, Ljungberg O, Ekberg O, Toth E. Cystic neuroendocrine tumor in the pancreas detected by endoscopic ultrasound and fine-needle aspiration: A case report. BMC Res Notes 2014;7:510. [CrossRef]
[Pubmed]

8.
Tremmel T, Holland-Cunz S, Günther P. Metastasized pancreatic neuroendocrine tumor in a teenage girl: A case report. J Med Case Rep 2015;9:230. [CrossRef]
[Pubmed]

9.
10.
Howell DL, O’Dorisio MS. Management of neuroendocrine tumors in children, adolescents, and young adults. J Pediatr Hematol Oncol 2012;34 Suppl 2:S64–68. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Dounia Najioullah - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ghizlane Laachir - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Latifa Chat - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Dounia Najioullah et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.