|
Case Report
Imaging findings of Müller–Weiss disease: A case report
1 Emergency Radiology Department, Ibn Sina Hospital, Rabat, Morocco
Address correspondence to:
Arthur Semedo Insumbo
Emergency Radiology Department, Ibn Sina Hospital, Rabat,
Morocco
Message to Corresponding Author
Article ID: 100014R02AI2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Insumbo AS, Sarah M, Jroundi FL, Laamrani FZ. Imaging findings of Müller–Weiss disease: A case report. Edorium J Radiol 2020;6:100014R02AI2020.ABSTRACT
Müller–Weiss disease is rare entity which is presumably post-traumatic osteonecrosis of the tarsal navicular bone in adults. In this article, we describ a radiographic and magnetic resonance imaging (MRI) findings of the disease in a 56-year-old female patient with bilateral tarsal pain, without any history of associated trauma. Physical examination revealed tenderness of mid-tarsal joint of each foot. Conservative treatment including non-weight bearing ambulation slightly improved the patient’s symptom. But an option of surgical treatment such as navicular fixation remains to be considered.
Keywords: Foot, Magnetic resonance imaging, Müller–Weiss disease, Navicular
INTRODUCTION
In 1927, Müller [1] described in adults a chronic deformity of the tarsal navicular bone due to forceful compression. In 1929, Weiss [2] also reported a similar disorder and claimed that osteonecrosis was the primary causative factor of the disorder. The disease is uncommon but has been known as Müller–Weiss disease (MWD) or syndrome which is associated with chronic midfoot pain. It often occurs in bilateral navicular bones of female patients [1],[2],[3],[4] and is characterized by progressive navicular fragmentation and talonavicular destruction [5],[6],[7],[8],[9],[10],[11],[12]. Müller–Weiss disease is often misdiagnosed or delayed diagnosed because it may be not familiar with clinicians.
In this article, we report a case with MWD describing radiographic and magnetic resonance imaging (MRI) findings.
CASE REPORT
A 56-year-old female patient, 1.64 meters tall and weighing 86 kg, who had complained pain in bilateral feet for one year, visited our trauma unit because of exacerbation of the symptomatology. She had no history of trauma. Physical examination demonstrated tenderness on mid-tarsal joint of each foot. A complete blood count was also unremarkable.
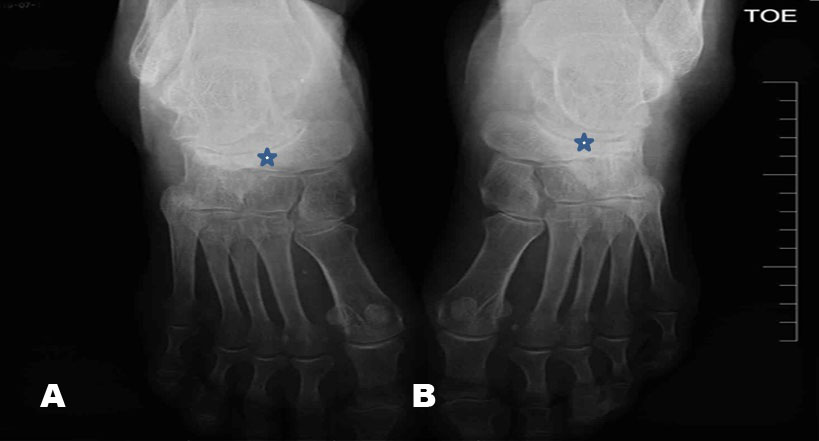
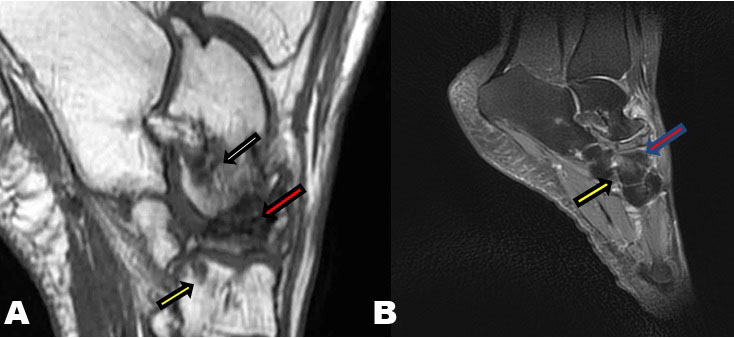
Radiographs of each foot were obtained for evaluation of midfoot pain. Sclerotic changes in the navicular bones were clearly shown on the lateral radiographs without obvious fractures (Figure 1). The anteroposterior view of each foot radiographs showed so-called “comma”-shaped deformity in the navicular bone with the medial displacement (Figure 2). The deformity which was due to collapse of the lateral portion of each navicular bone was predominantly shown in the right one. The patient underwent MRI with various sequences to evaluate the sclerotic navicular bones, and showed a collapse of the left navicular bone with normal cortical bone, and severe collapse of the right navicular bone with a disruption of cortical bone (Figure 3 and Figure 4). The anterior portion of the right talus had bone marrow edema with hyperintensity on fat suppressed images due to the talonavicular joint osteoarthrosis. Both radiographic and MRI findings, combined with the patient’s history and clinical findings, were compatible with MWD involving bilateral navicular bones.
Anti-inflammatory drugs orally, conservative treatment including weight reduction with non-weight bearing ambulation slightly improved the patient’s symptom.
An ulterior surgical navicular fixation was performed with a good outcome. The differential diagnosis for spontaneous tarsal osteonecrosis includes pathologies as follows:
- Mechanically induced stress-adaptive sclerosis
- Callus formation related to insufficiency fracture
- Healing of acute traumatic fracture
On direct surgical inspection, there was no evidence of malodor or purulence, the possibility of osteomyelitis was not found.
DISCUSSION
Müller–Weiss disease is a rare disease that appears most often in women over 40 years of age, and which has been described and characterized by compression of the navicular bone situated between talus and the lateral cuneiform bone resulting in spontaneous osteonecrosis of the navicular bone causing severe foot pain and bone deformity [12].
Müller–Weiss disease is usually diagnosed by imaging findings associated with clinical history. Most patients present with chronic midfoot pain in the fourth or fifth decades. The bilateral distribution in middle-aged women is a characteristic of the disease as this reported case. However, unilateral changes may be evident in younger individuals [1],[2],[3],[4],[5],[6],[7],[8],[9],[10],[11],[12]. With further navicular collapse, secondary osteoarthrosis develops. The radiographic abnormalities of MWD are represented as primary osteonecrosis of the tarsal navicular bone. Initial alterations include a loss of volume in the lateral portion of the tarsal navicular with increasing radiopacity. The changes result in a comma-shaped deformity due to collapse of the lateral half of the bone [6],[7],[8],[9],[10],[11]. Peritalar subluxation may also occur in the medial aspect of the navicular and causing a new articulation [5]. Subsequently in the same way, dorsal protrusion and fragmentation of the bone could also often be seen [1].
Magnetic resonance imaging can detect bone marrow edema and early osteoarthrosis changes and exclude other differential diagnosis [13], such as stress fracture which frequently occurs in the navicular. Stress fractures usually originate at the dorsal, proximal cortex of the navicular and progress distally to the plantar surface [6]. Repetitive stress injury as bone marrow edema can be seen on MRI. However, it may be difficult to differentiate the primary osteonecrosis from the secondary osteonecrosis caused by long-term complication of stress fracture [6],[14]. Osteomyelitis with periosteal and soft tissue lesions can also be excluded by MRI. Magnetic resonance imaging can easily detect talar osteoarthrosis with a disappearance of the articular talonavicular space and marginal osteophytes in MWD. Koehler disease in which radiographic and MRI findings are similar to MWD is self-limited osteonecrosis of navicular in child under six years [15].
The middle-aged women with bilateral navicular osteonecrosis are preferred to MWD [1], although unilateral navicular lesion may be evident in younger individuals in the disease [3]. The osteonecrosis in MWD is categorized as spontaneous although some authors are thought to be presumably post-traumatic osteonecrosis [6]. It is not clear whether previous injury or chronic stress is the primary cause of spontaneous osteonecrosis. Radiographs, MRI or CT alone cannot distinguish spontaneous osteonecrosis of the tarsal navicular secondary osteonecrosis due to rheumatoid arthritis, renal failure, and lupus erythematosus [7],[8],[9],[10],[11],[12].
Osteonecrosis or avascular osteonecrosis is caused by disruption of the bone’s vascular supply [16],[17],[18]. The dorsal aspect of the navicular [8] is supplied by branches from the dorsal pedis artery, whereas the plantar aspect is supplied by the medial plantar artery, and the central third of the navicular, tension forces on the plantar aponeurosis increase with ventral shifting of weight during loading, as occurs in association with pes planus. Simultaneous increase in pressure within the marrow of the tarsal navicular could lead to inadequacy of blood flow to its lateral portion. Ligamentous laxity, giving rise to protrusion of the bone, may further compromise the blood supply by injuring the radially distributed vessels that enter the circumference of the tarsal navicular [9],[10].
Müller–Weiss disease can lead to advanced midtarsal osteoarthritis and subsequent permanent disability [7]. Treatment of MWD generally consists of non-weight-bearing cast immobilization and oral anti-inflammatory and analgesic medication but requires surgical fixation using bone graft [5].
CONCLUSION
Müller–Weiss disease should be considered in middle-aged patients with unexplained mid-foot pain. The disease can result in disability and deformity; however, a better understanding of this disease and its radiologic manifestations may allow earlier diagnosis and improve future management.
REFERENCES
1.
Fernández de Retana P, Maceira E, Fernández-Valencia JA, Suso S. Arthrodesis of the talonavicular-cuneiform joints in Müller-Weiss disease. Foot Ankle Clin 2004;9(1):65–72. [CrossRef]
[Pubmed]

2.
Hetsroni I, Nyska M, Ayalon M. Plantar pressure distribution in patients with Müller-Weiss disease. Foot Ankle Int 2007;28(2):237–41. [CrossRef]
[Pubmed]

3.
Janositz G, Sisák K, Tóth K. Percutaneous decompression for the treatment of Mueller-Weiss syndrome. Knee Surg Sports Traumatol Arthrosc 2011;19(4):688–90. [CrossRef]
[Pubmed]

4.
Lui TH. Arthroscopic triple arthrodesis in patients with Müller Weiss disease. Foot Ankle Surg 2009;15(3):119–22. [CrossRef]
[Pubmed]

5.
Fuentealba A, Butrón S, Drewes J, et al. Müller Weiss syndrome: A forgotten cause of mid foot pain. A multimodality pictorial review. ECR 2017. [CrossRef]

6.
7.
Tosun B, Al F, Tosun A. Spontaneous osteonecrosis of the tarsal navicular in an adult: Mueller-Weiss syndrome. J Foot Ankle Surg 2011;50(2):221–4. [CrossRef]
[Pubmed]

8.
Scott-Moncrieff A, Forster BB, Andrews G, Khan K. The adult tarsal navicular: Why it matters. Can Assoc Radiolo J 2007;58(5):279–28.
[Pubmed]

9.
Haller J, Sartoris DJ, Resnick D, et al. Spontaneous osteonecrosis of the tarsal navicular in adults: Imaging findings. AJR Am J Roentgenol 1988;151(2):355–8. [CrossRef]
[Pubmed]

10.
Sarrafian SK. Functional characteristics of the foot and plantar aponeurosis under tibiotalar loading. Foot Ankle 1987;8(1):4–18. [CrossRef]
[Pubmed]

11.
Kani KK. Mulcahy H, Chew FS. Case 228: Muller-Weiss disease. Rediology 2016;279(1):317–21. [CrossRef]
[Pubmed]

12.
Gillespy T 3rd, Genant HK, Helms CA. Magnetic resonance imaging of osteonecrosis. Radiol Clin North Am 1986;24(2):193–208.
[Pubmed]

13.
Scoles PV, Yoon YS, Makley JT, Kalamchi A. Nuclear magnetic resonance imaging in Legg-Calvé-Perthes disease. J Bone Joint Surg Am 1984;66(9):1357–63.
[Pubmed]

14.
Manter JT. Distribution of compression forces in the joints of the human foot. Anat Rec 1946;96(3):313–21. [CrossRef]
[Pubmed]

15.
Waugh W. The ossification and vascularization of the tarsal navicular and their relations to Köhler’s disease. J Bone Joint Surg Br 1958;40-B(4):765–77.
[Pubmed]

16.
Sierra A, Potchen EJ, Moore J, Smith HG. High-field magnetic-resonance imaging of aseptic necrosis of the talus: A case report. J Bone Joint Surg Am 1986;68(6):927–8.
[Pubmed]

17.
Hatoff A. Bipartite navicular bone as a cause of flatfoot. AMA Am J Dis Child 1950;80(6):991–2. [CrossRef]
[Pubmed]

18.
Mau H. On the knowledge of os naviculare bipartitum pedis. [Article in German]. Z Orthop Ihre Grenzgeb 1960;93:404–10.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Arthur Semedo Insumbo - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Moumna Sarah - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
F L Jroundi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
F Z Laamrani - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Arthur Semedo Insumbo et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.