|
Case Report
Alternating hemiplegia revealing a vertebrobasilar dolichoectasia: A case report and review of the literature
1 Military Hospital, Radiology Department, Mohamed V University, Rabat, Morocco
Address correspondence to:
Fabrice Diekouadio
Military Hospital, Mohamed V University, Rabat,
Morocco
Message to Corresponding Author
Article ID: 100013R02FD2019
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Diekouadio F, El Bakkari A, Ayouche O, Mohamed DA, Chaoui B. Alternating hemiplegia revealing a vertebrobasilar dolichoectasia: A case report and review of the literature. Edorium J Radiol 2019;5:100013R02FD2019.ABSTRACT
Introduction: Vertebrobasilar dolichoectasia (VBD) is defined by an increase in the length and size of vertebrobasilar system, which take on a tortuous aspect. This pathology is due to a rarefaction of the internal elastic lamina at the media level of the dolichoectatic artery. Vertebrobasilar dolichoectasia is usually asymptomatic and can be discovered by chance. In symptomatic patients, the clinical signs may be due to three factors: ischemic complications, hemorrhagic or signs of compression of the brain stem, cranial nerves or third ventricle.
Case Report: Here we describe the case of a 67-year-old man who presented with left hemiparesis with ophthalmoplegia and right peripheral facial palsy. These clinical signs suggested an alternating hemiplegia, indicating brain stem involvement. As part of the evaluation, he received a brain scan and magnetic resonance imaging (MRI) of the brain with magnetic resonance angiography (MRA), which revealed the presence of basilar artery dolichoectasia. Current diagnostic criteria for computed tomography (CT) and MRI scans include three quantitative measurements of basilar dolichoectasia: lateral score, bifurcation height, and basilar artery diameter.
Conclusion: Dolichoectasia is an unusual vasculopathy that causes enlargement, tortuosity, or lengthening of the arteries. Intracranial arterial dolichoectasia most often involves the vertebrobasilar system. Ischemic strokes are the most common, followed by progressive compression of the cranial nerves and brain stem, cerebral hemorrhage, and hydrocephalus. In our case, VBD has caused an alternating syndrome.
Keywords: Alternating hemiplegia, Dolichoectasia, Vertebrobasilar
INTRODUCTION
The term dolichoectasia (derived from the Greek words dolichos meaning “abnormally long” and ektasis meaning “dilation”) is used to describe a dilated, elongated, and tortuous appearance. Vertebrobasilar dolichoectasia (VBD) therefore defines a tortuous dilatation of the vertebrobasilar system [1]. It is a rare arterial disease, responsible for hemostatic, hemodynamic, and signs of compression, which can lead to posterior cerebral ischemia, intracranial hemorrhage, neurological disorders, or hydrocephalus. Vertebrobasilar dolichoectasia may, however, remain asymptomatic and to be discovered by chance [2]. The severity of the symptoms is usually related to the age of the patient and the location of the lesions. The alternating hemiplegia is defined by the presence of signs of involvement of one or more cranial nerves on the same side as the lesion, and signs of involvement of a long, pyramidal, sensitive, or cerebellar pathway on the opposite side to the lesion.
CASE REPORT
Our case is about a 67-year-old chronic smoker, followed for high blood pressure under Nicardipine, hospitalized following the abrupt onset of left hemiparesis, associated with right peripheral ophthalmoplegia and facial paralysis. He was afebrile and his blood pressure was 16/10.
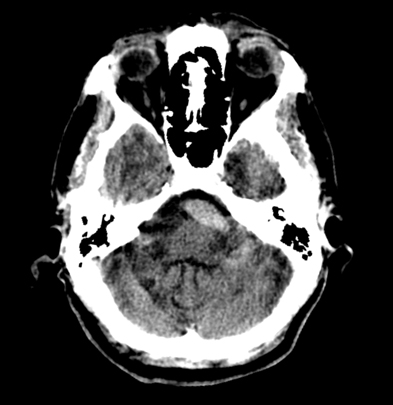
The biological assessment (sedimentation rate, blood count, blood glucose, and C-reactive protein) was normal. A brain scan without contrast injection performed revealed a spontaneously hyperdense aspect of the basilar artery, which had significant ectasia with a tortuous appearance, without associated parietal calcification (Figure 1). An angio-MRI was performed for a better characterization of the dolichoectasia and to explore the compression of the nerves.
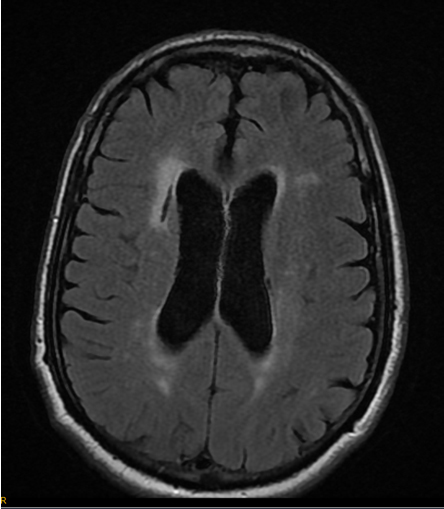
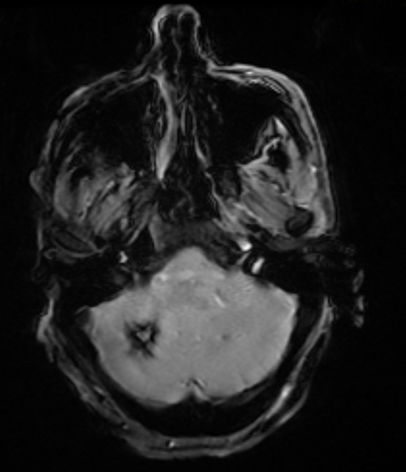
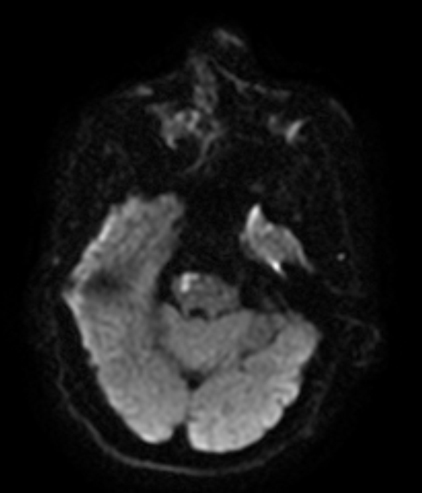
The MRI reported signal abnormalities of the periventricular white matter in hyperintensity T2 and FLAIR suggestive of leukoaraiosis, associated with a lacunary image facing the anterior horn of the right lateral ventricle in relation to a sequelar ischemia (Figure 2).
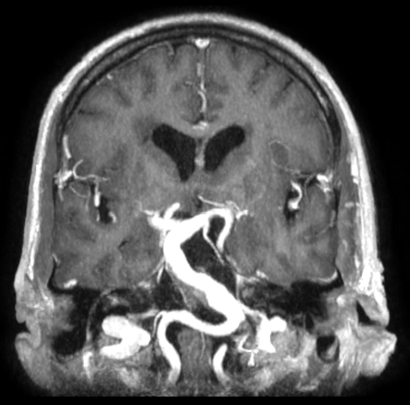
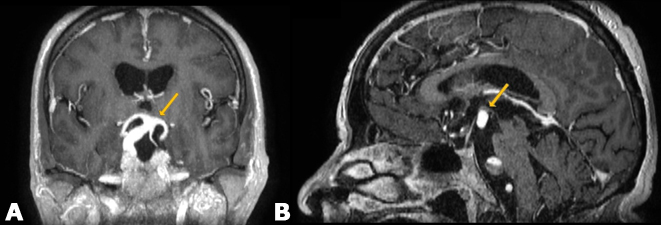
On the subtemporal floor, MRI better defined the ectasia of the entire basal artery, measured at 8 mm in diameter, with a tortuous appearance (Figure 3).
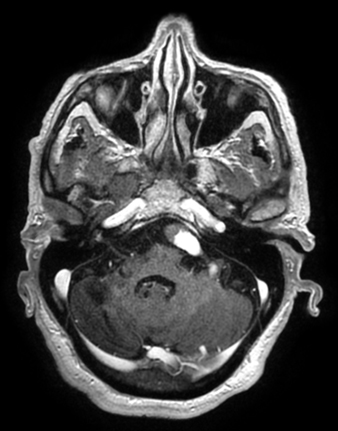
He associated a partial thrombosis localized to its lower part, extended on 13 mm (Figure 4).
At the level of the cerebellum, there was an inferior right anterolateral hemisphere lesion in heterogeneous T2-weighted hyperintensity, with hyposignal T2* shell in relation to hemorrhagic softening of an ischemic lesion (Figure 5).
At the brain stem level, MRI revealed T2-weighted hyperintensity and right anterolateral pontic diffusion in relation to a recent ischemic stroke (Figure 6). We found no sign of a dilated ventricle.
DISCUSSION
Intracranial arterial dolichoectasias are infrequent vascular lesions, resulting in dilatation, tortuosity, and lengthening of one or more intracranial arteries.
The vertebrobasilar system is more frequently affected than the anterior intracranial vasculature. The prevalence in the adult population is estimated at 0.06–5.8% [3].
The physiopathology of the VBD is still the subject of several hypotheses; however, factors such as trophic support depletion, degeneration of the internal elastic lamina, reticular fiber deficiency, and atrophy of the smooth muscle of the dolichoectatic artery may explain the occurrence of dolichoectasias [4].
Vertebrobasilar dolichoectasia can have a congenital origin (Marfan’s syndrome, Ehlers–Danlos syndrome) or acquired one (atherosclerosis) [5]. Alternating hemiplegia is a form of stroke with involvement of one or more cranial nerves on the side of the lesion and pyramidal or cerebellar involvement on the opposite side to the lesion.
It is explained by ischemia of the brain stem, consecutive to the occlusion of the paramedian branches of the posterior cerebral artery or perforating arteries of the basilar trunk.
Clinic
Vertebrobasilar dolichoectasia is often asymptomatic (40% of cases) [6]. Arterial ectasia leads hemodynamic disorders (slowing of blood flow by decreasing anterograde flow, as well as a decrease in mean systolic velocity, and turbulence by the appearance of a retrograde flow), which will be responsible for recurrent thrombosis, which is likely to send fibrinocruoric microemboli locally or remotely and thus cause repeated cerebral ischemia.
Ischemic stroke is therefore the most common clinical manifestation of VBD [7]. It is characterized by posterior cerebral ischemia [8]. In our case, acute right pontic ischemia seems to be at the origin of the alternating hemiplegia.
Trophic disorders by rarefaction of the internal elastic lamina are responsible for the fragility of the dolichoectatic artery. The latter can therefore break and cause hemorrhagic stroke, or subarachnoid hemorrhage. The occurrence of subarachnoid hemorrhage may be facilitated by arterial hypertension and the use of anticoagulants or antiplatelet agents [9].
Vertebrobasilar dolichoectasia can cause compression of surrounding anatomical structures, including cranial nerves, brain stem, and third ventricle [10].
The compression of a cranial nerve is a frequent mode of revelation; most often incriminating a dolichoectatic basilar artery compressing the emergence of a cranial nerve in the brain stem. The facial nerve (VII) and the trigeminal nerve are the most frequently affected. Their involvement will respectively cause paralysis or hemifacial spasm, and trigeminal neuralgia.
The compression of the 8th pair of cranial nerves will result in a perception deafness or a vertiginous syndrome [11]. Oculomotor (III, IV, and VI) involvement is manifested by diplopia and ophthalmoplegia. The VBD can also compress the medulla oblongata, causing progressive ataxia and tetraparesis [12].
Compression of the third ventricle is rare. It is manifested by hydrocephalus, which is responsible for an intracranial hypertension syndrome. This hydrocephalus has two mechanisms: the compression of the floor of the third ventricle and the phenomenon of back pressure (hammer effect) generated by the beats of the dolichoectatic artery [13].
Imaging
CT scan
A first acquisition without contrast agent is important to first look for calcifications within the wall of the dolichoectatic artery. This sign is common in the VBD. The dolichoectatic artery can also take on a spontaneously hyperdense appearance.
Computed tomography can also show the mechanisms responsible for clinical signs in case of VBD: Cerebral ischemia (intraparenchymal hypodense range of arterial systemization), meningeal hemorrhage (spontaneous hyperdensity of subarachnoid spaces), mass effect on the third ventricle and brain stem.
After injection of contrast agent, we visualize the dilated and tortuous aspect of the vertebrobasilar system.
Magnetic resonance angiography
This examination is more sensitive than the scanner in the diagnosis of VBD [14]. The angio-MRI allows a better visualization of dolichoectasia; it is called ectasia when the diameter of the basilar artery is greater than 4.5 mm [15]. Time-of-flight (TOF) MRA provides excellent VBD analysis. Smoker et al. established diagnostic criteria by angio-CT and MRI for the VBD, to assess the degree of dolichoectasia [16].
These criteria include three quantitative measures of basilar artery morphology:
Laterality score and height of bifurcation as measures of assessment of tortuosity and lengthening, and basilar artery diameter for ectasia. The height of the basilar artery and the degree of laterality are classified from 0 to 3.
The degree of laterality of the basilar artery is measured on the axial sections (0: midline, 1: within the lateral edge of the clivus or dorsum sellae, 2: outside the lateral edge of the clivus or dorsum sellae, and 3: in the cerebellopontine angular cistern). In our case, it is a grade 2 (Figure 4). The position of the basal trunk is considered normal if it lies within the lateral border of the clivus or dorsum sellae throughout its course [17].
Measuring the height of the bifurcation of the basilar artery makes it possible to evaluate the length of the basilar trunk: (0: at or below the sellae dorsum, 1: in the suprasellar cistern, 2: at the level of the floor of the third ventricle, and 3: indentation and elevation of the floor of the third ventricle). In our case, it is a grade 3 (Figure 7).
The angio-MRI also allows a good visualization of the arterial lumen and thus to search for endoluminal thromboses. It allows to look for signs of compression of the brain stem, cranial pairs, and the third ventricle. It also reveals signs of ischemia in the vertebral basilar territory and subarachnoidal or intraparenchymal hemorrhage.
Arteriography
Cerebral arteriography is an invasive examination that allows visualization of the arterial lumen.
It allows highlighting the lengthening and ectasia of the basilar artery.
It has more disadvantages than MRI because of the invasive nature and the risk of transient vertebrobasilar or definitive postarteriographic ischemia [18].
Treatment
The triple evolutionary potential (thromboembolism, rupture, and compression) makes the therapeutic choice delicate. The treatment of VBD is therefore both medical (prevention of ischemia and cerebral hemorrhage) and surgical (decompressive treatment in case of vasculonervous conflict, endovascular treatment). The artery in question is most often a dolichoectatic basilar artery. The decompressive surgical treatment gives good results [19].
CONCLUSION
Intracranial dolichoectasia is a vascular disease characterized by a tortuous dilatation of the intracranial arteries. Its most common clinical manifestations include strokes, which most often involve areas vascularized by the arteries of the vertebrobasilar system; therefore, it is necessary to discuss this etiology in front of a patient with an alternating hemiplegia.
REFERENCES
1.
Pham T, Wesolowski J, Trobe JD. Sixth cranial nerve palsy and ipsilateral trigeminal neuralgia caused by vertebrobasilar dolichoectasia. Am J Ophthalmol Case Rep 2018;10:229–32. [CrossRef]
[Pubmed]

2.
Shapiro M, Becske T, Riina HA, Raz E, Zumofen D, Nelson PK. Non-saccular vertebrobasilar aneurysms and dolichoectasia: A systematic literature review. J Neurointerv Surg 2014;6(5):389–93. [CrossRef]
[Pubmed]

3.
Baran B, Kornafel O, Guziński M, Sąsiadek M. Dolichoectasia of the circle of Willis arteries and fusiform aneurysm of basilar artery – case report and review of the literature. Pol J Radiol 2012;77(2):54-9.
[Pubmed]

4.
Hegedüs K. Ectasia of the basilar artery with special reference to possible pathogenesis. Surg Neurol 1985;24(4):463–9.
[Pubmed]

5.
Passero SG, Rossi S. Natural history of vertebrobasilar dolichoectasia. Neurology 2008;70(1):66–72. [CrossRef]
[Pubmed]

6.
de Oliveira Rde M, Cardeal JO, Lima JG. Basilar ectasia and stroke: Clinical aspects of 21 cases. [Article in Portuguese]. Arq Neuropsiquiatr 1997;55(3B):558–62.
[Pubmed]

7.
Flemming KD, Wiebers DO, Brown RD Jr, et al. The natural history of radiographically defined vertebrobasilar nonsaccular intracranial aneurysms. Cerebrovasc Dis 2005;20(4):270–9. [CrossRef]
[Pubmed]

8.
9.
Takeuchi S, Takasato Y, Masaoka H, et al. Dolichoectasia involving the vertebrobasilar and carotid artery systems. J Clin Neurosci 2009;16(10):1344–6. [CrossRef]
[Pubmed]

10.
Savitz SI, Ronthal M, Caplan LR. Vertebral artery compression of the medulla. Arch Neurol 2006;63(2):234–41. [CrossRef]
[Pubmed]

11.
Kerber CW, Margolis MT, Newton TH. Tortuous vertebrobasilar system: A cause of cranial nerve signs. Neuroradiology 1972;4(2):74–7.
[Pubmed]

12.
Hongo K, Kobayashi S, Hokama M, Sugita K. Vertebral artery section for treating arterial compression of the medulla oblongata. Case report. J Neurosurg 1993;79(1):116–8. [CrossRef]
[Pubmed]

13.
Breig A, Ekbom K, Greitz T, Kugelberg E. Hydrocephalus due to elongated basilar artery: A new clinicoradiological syndrome. Lancet 1967;1(7495):874–5. [CrossRef]
[Pubmed]

14.
Rautenberg W, Aulich A, Röther J, Wentz KU, Hennerici M. Stroke and dolichoectatic intracranial arteries. Neurol Res 1992;14(42 Suppl):201–3.
[Pubmed]

15.
Lou M, Caplan LR. Vertebrobasilar dilatative arteriopathy (dolichoectasia). Ann N Y Acad Sci 2010;1184:121–33. [CrossRef]
[Pubmed]

16.
Samim M, Goldstein A, Schindler J, Johnson MH. Multimodality imaging of vertebrobasilar dolichoectasia: Clinical presentations and imaging spetrum. Rradiographics 2016;36(4):1129–46. [CrossRef]
[Pubmed]

17.
Smoker WR, Price MJ, Keyes WD, Corbett JJ, Gentry LR. High-resolution computed tomography of the basilar artery: 1. Normal size and position. AJNR Am J Neuroradiol 1986;7(1):55–60.
[Pubmed]

18.
Smoker WR, Corbett JJ, Gentry LR, Keyes WD, Price MJ, McKusker S. High-resolution computed tomography of the basilar artery: 2. Vertebrobasilar dolichoectasia: Clinical-pathologic correlation and review. AJNR Am J Neuroradiol 1986;7(1):61–72.
[Pubmed]

19.
Linskey ME, Jho HD, Jannetta PJ. Microvascular decompression for trigeminal neuralgia caused by vertebrobasilar compression. J Neurosurg 1994;81(1):1–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Fabrice Diekouadio - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Asaad El Bakkari - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Othman Ayouche - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Daoud Ali Mohamed - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Badr Chaoui - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2019 Fabrice Diekouadio et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.