|
Case Report
MR imaging findings in children with merosin-deficient congenital muscular dystrophy
1 Resident of Radiology, Faculty of Medicine and Pharmacies of Rabat, Medical Imaging Services for Maternity and Children – University Hospital Center IBN SINA – Rabat, Morocco
2 Assistant Professor of Radiology, Faculty of Medicine and Pharmacies of Rabat, Medical Imaging Services for Maternity and Children – University Hospital Center IBN SINA – Rabat, Morocco
3 Chief of the Medical Imaging Services for Maternity and Children – University Hospital Center IBN SINA – Rabat, Morocco
4 Professor of Radiology, Faculty of Medicine and Pharmacies of Rabat, Medical Imaging Services for Maternity and Children – University Hospital Center IBN SINA – Rabat, Morocco
Address correspondence to:
Arthur Semedo Insumbo
Rabat,
Morocco
Message to Corresponding Author
Article ID: 100019R02AI2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Insumbo AS, El Yousfi Z, El Haddad S, Chat L, Allali N. MR imaging findings in children with merosindeficient congenital muscular dystrophy. Edorium J Radiol 2021;7:100019R02AI2021.ABSTRACT
Congenital muscular dystrophy (CMD) constitutes a set of diseases which differ, sometimes very much from each other. Congenital muscular dystrophy also known as a heterogeneous group of disorders with muscle weakness, hypotonia, and contractures present at birth. This disease is essentially characterized by a complete absence of merosin. Brain magnetic resonance imaging (MRI) in children the lesions presenting with high signal intensities are often observed throughout the centrum semi-oval, periventricular, and sub-cortical white matters on T2-weighted images in MRI brain in children with merosin-deficient congenital muscular dystrophy (MDCMD). In several studies it is noted that the apparent diffusion coefficient (ADC) map may reveal increased signal intensity and at the same times it may value in the periventricular and deep white matters. In this case report we would like to demonstrate the brain MRI characteristics of MDCMD in a young child of 15 years old.
Keywords: Congenital muscular dystrophy, MRI, White-matter abnormalities
INTRODUCTION
Congenital muscular dystrophy (CMD) defined as a group of mixed disorders that present at birth which is essentially characterized by muscle weakness, hypotonia, and contractures.
A dystrophic pattern is usually always confirmed in muscle biopsy specimens [1],[2]. The CMD has been classified in two forms well-recognized. The classic or pure form of CMD is seen in patients with normal or near-normal intelligence. The second one differs from the classic or pure form in that brain anomalies and severe mental retardation are present [2]. This second group includes other variants described in the Japanese medical science known as Fukuyama CMD, the Walker-Warburg syndrome, and the Santavuori syndrome (muscle-eye-brain disease) [3].
It is important to remember that Fukuyama, Walker-Warburg, and Santavuori syndromes both have a variety of neuro-pathologic abnormalities that include abnormal cerebral and cerebellar gyral patterns, cerebellar cysts, and white matter changes on MR images [2],[3],[4],[5],[6],[7],[8],[9]. The white matter findings are observed in late infancy and with a tendency to decrease in severity with age [2],[3],[4],[5],[6],[7],[8],[9]. The pathogenesis of these changes still unclear and remains uncertain at this time. In some investigations imaging findings in the pure form of CMD have recently been reported, along with their association with abnormal sensory and visual evoked potentials [6],[7],[10].
We outline the specific MRI findings seen in patients hospitalized in one of the pediatric hospitals in the kingdom of Morocco late diagnosed with documented MDCMD.
CASE REPORT
A 15-year-old boy, weighed 37.5 kg, presented to us with isolated delayed motor milestones noticed in early infancy. His parents noted a head lag at 4-month-old and subsequent delay in attaining other motor milestones.
He was able to sit and stand only with support and was not able to walk. Although there is a slight defect in memory capacity, his mental ability and speech appeared to be normal. Vision and hearing were normal. There was no history of seizures. No respiratory difficulty was noted. His birth and family history were unremarkable. On examination, his vital signs were normal. He had classical myopathic facies with inverted “v”-shaped upper lip and shallow cheeks. There were no other dysmorphic features. With these clinical data the CDM was suspected and later confirmed by the MRI.
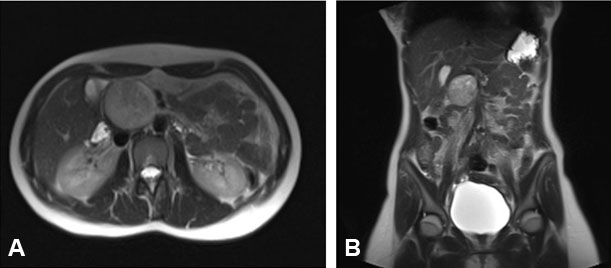
Brain magnetic resonance imaging (MRI) showed diffuse and symmetrical increase in T2W signal in white matter of cerebral hemispheres (Figure 1A). And also brain stem and cerebellum showed abnormally in increasing signal. Ventricles were not dilated. The major abnormality was abnormal T2 prolongation in cerebral white matter, without involvement of corpus callosum, internal capsule, or other structural abnormalities. Signal characteristic of corpus callosum, internal capsule, basal ganglia, and thalami were normal (not showed). Diffusion weighted imaging (DWI) demonstrated no evidence of restricted diffusion.
DISCUSSION
Merosin (also called α2 laminin) is an extracellular matrix protein, whose gene is mapped in the chromosome 6p2. Laminins are a family of proteins of the basement membrane, and the predominant laminin variant in the basement membrane of the adult striated muscle is the merosin (α2 laminin), which is expressed in skeletal muscle, Schwann cells, cardiac muscle, and placental villi.
Merosin binds α-dystroglycan and in turn is linked to the subsacrolemmal cytoskeleton via the dystrophin-glycoprotein complex. The deficiency of this protein can condition an interruption of the connection between the matrix extracellular tissue and the cytoskeleton subsarcolemma, muscle degeneration [11],[12]. Merosin also plays an important role in neuronal migration and precursors of oligodendrocytes [13],[14].
Some recent studies findings have suggested that myofiber injury may be the result of an inflammatory attack on muscle, followed by poor regeneration of myofibers caused mainly by a defective basal lamina [15]. Merosin is expressed in the fetal brain and its deficiency must be related to changes in white matter and with anomalies of cortical development [16].
Generally in the clinical evaluation of patients with MDCMD is possible to find congenital hypotonia and weakness, and, in late infancy, have contractures and delayed motor milestones.
Nevertheless, the clinical conditions, the patients are able to improve their health status if they survive past the neonatal period, their neuromuscular condition stabilizes and also they may have normal or near-normal intelligence as in our patient.
In this article, we describe the clinical changes and imaging findings of a 15-year-old patient with MDCMD. The patient has normal intelligence, epilepsy, and marked changes in the substance sign supra and infratentorial white matter, associated with global atrophy (Figure 1B) of the pons or cerebellum and brain stem, and small subcortical cerebellum cystic cavitation (Figure 2A and Figure 2B).
The MRI finding was similar with the study described about three children by Pilar et al. [17]. On T2-weighted image, the patient had a diffuse and symmetrical increase in signal in the white matter of the cerebral hemispheres, same alterations of the normal white matter signal in the cerebellum, there were also evidence of white matter subcortical cerebellum cysts cavitation, global atrophy of the pons or cerebellum and brain stem, and no evidence of structural abnormalities, such as focal occipital agyria, and enlarged lateral ventricles. The signal characteristic of the white matter within the corpus callosum, internal capsule was normal in our patient.
Many changes seen in the white matter in our patient were similar to those described in the literature that there was progression of white matter disease [10]. Trevisan et al. describe one patient with MDCMD, whose imaging studies from age 2 months to 5 years showed progression of leukoencephalopathy [10].
In our patient there was no historical data of his childhood about the disease, but everything indicates to be followed for years.
Philpot described an 11-year-old child, disabled in merosin, with moderate mental retardation and epilepsy of difficult control, whose brain MRI revealed marked bilateral occipital agyria, dot-cerebellar, and mild hypoplasia dilation of the lateral ventricles [13].
On the other hand it is important to say that it is known, however, that merosin promotes neurite outgrowth and Schwann cell migration, this fact was described by Engvall and Tan et al. [18],[19],[20]. In the brain, merosin has been found in the basement membrane of blood vessels [20]. Villanova et al. postulated that this may result in an alteration in the blood-brain barrier, leading to vascular hyperpermeability and the penetration of substances into the central nervous system (CNS) [21].
CONCLUSION
This case has demonstrated the manifestations of merosin deficiency through clinical presentations and MRI findings. It is extremely important to emphasize that MR plays a very important role in confirming the diagnosis of MDCMD. In many studies the conclusions reached have revealed that subtle changes in the white matter may be seen in early infancy and aid in the diagnosis of CMD. Therefore, if changes in white matter are not seen in early childhood, due to lack of resources or other reasons, a repeated study in early childhood or in a young child (like our patient) can also be revealing and help confirm the diagnosis in a child with characteristic of CMD with merosin deficiency. Furthermore, our case recalls the possible CNS involvement in merosin-deficient patients, at least that we suggest to perform MRI for all patients with non-MDCMD.
REFERENCES
1.
Tomé FM, Evangelista T, Leclerc A, et al. Congenital muscular dystrophy with merosin deficiency. C R Acad Sci III 1994;317(4):351–7.
[Pubmed]

2.
Leyten QH, Gabreëls FJ, Renier WO, et al. White matter abnormalities in congenital muscular dystrophy. J Neurol Sci 1995;129(2):162–9. [CrossRef]
[Pubmed]

3.
Trevisan CP, Martinello F, Ferruzza E, Angelini C. Divergence of central nervous system involvement in 2 Italian sisters with congenital muscular dystrophy: A clinical and neuroradiological follow-up. Eur Neurol 1995;35(4):230–5. [CrossRef]
[Pubmed]

4.
Trevisan CP, Carollo C, Segalla P, Angelini C, Drigo P, Giordano R. Congenital muscular dystrophy: Brain alterations in an unselected series of Western patients. J Neurol Neurosurg Psychiatry 1991;54(4):330–4. [CrossRef]
[Pubmed]

5.
Aida N, Tamagawa K, Takada K, et al. Brain MR in Fukuyama congenital muscular dystrophy. AJNR Am J Neuroradiol 1996;17(4):605–13.
[Pubmed]

6.
Mercuri E, Muntoni F, Berardinelli A, et al. Somatosensory and visual evoked potentials in congenital muscular dystrophy: Correlation with MRI changes and muscle merosin status. Neuropediatrics 1995;26(1):3–7. [CrossRef]
[Pubmed]

7.
Reed UC, Marie SK, Vainzof M, et al. Congenital muscular dystrophy with cerebral white matter hypodensity. Correlation of clinical features and merosin deficiency. Brain Dev 1996;18(1):53–8. [CrossRef]
[Pubmed]

8.
Nogen AG. Congenital muscle disease and abnormal findings on computerized tomography. Dev Med Child Neurol 1980;22:658–63. [CrossRef]
[Pubmed]

9.
Yoshioka M, Kuroki S, Mizue H. Congenital muscular dystrophy of non-Fukuyama type with characteristic CT images. Brain Dev 1987;9(3):316–8. [CrossRef]
[Pubmed]

10.
Trevisan CP, Martinello F, Ferruzza E, Fanin M, Chevallay M, Tomé FM. Brain alterations in the classical form of congenital muscular dystrophy. Clinical and neuroimaging follow-up of 12 cases and correlation with the expression of merosin in muscle. Childs Nerv Syst 1996;12(10):604–10. [CrossRef]
[Pubmed]

11.
Ibraghimov-Beskrovnaya O, Ervasti JM, Leveille CJ, Slaughter CA, Sernett SW, Campbell KP. Primary structure of dystrophin-associated glycoproteins linking dystrophin to the extracellular matrix. Nature 1992;355(6362):696–702. [CrossRef]
[Pubmed]

12.
Ervasti JM, Campbell KP. A role for the dystrophinglycoprotein complex as a transmembrane linker between laminin and actin. J Cell Biol 1993;122(4):809–23. [CrossRef]
[Pubmed]

13.
Philpot J, Cowan F, Pennock J, Sewry C, Dubowitz V, Bydder G, Muntoni F. Merosin-deficient congenital muscular dystrophy: The spectrum of brain involvement on magnetic resonance imaging. Neuromuscul Disord 1999;9(2):81–5. [CrossRef]
[Pubmed]

14.
Barkovich AJ. Neuroimaging manifestations and classification of congenital muscular dystrophies. AJNR Am J Neuroradiol 1998;19(8):1389–96.
[Pubmed]

15.
Pegoraro E, Mancias P, Swerdlow SH, et al. Congenital muscular dystrophy with primary laminin alpha2 (merosin) deficiency presenting as inflammatory myopathy. Ann Neurol 1996;40(5):782–91. [CrossRef]
[Pubmed]

16.
Mackay MT, Kornberg AJ, Shield L, et al. Congenital muscular dystrophy, white-matter abnormalities, and neuronal migration disorders: The expanding concept. J Child Neurol 1998;13(10):481–7. [CrossRef]
[Pubmed]

17.
Caro PA, Scavina M, Hoffman E, Pegoraro E, Marks HG. MR imaging findings in children with merosindeficient congenital muscular dystrophy. AJNR Am J Neuroradiol 1999;20(2):324–6.
[Pubmed]

18.
Engvall E, Davis GE, Dickerson K, Ruoslahti E, Varon S, Manthorpe M. Mapping of domains in human laminin using monoclonal antibodies: Localization of the neurite-promoting site. J Cell Biol 1986;103(6 Pt 1):2457–65. [CrossRef]
[Pubmed]

19.
Engvall E, Earwicker D, Day A, Muir D, Manthorpe M, Paulsson M. Merosin promotes cell attachment and neurite outgrowth and is a component of the neurite-promoting factor of RN22 schwannoma cells. Exp Cell Res 1992;198(1):115–23. [CrossRef]
[Pubmed]

20.
Tan E, Topaloglu H, Sewry C, et al. Late onset muscular dystrophy with cerebral white matter changes due to partial merosin deficiency. Neuromuscul Disord 1997;7(2):85–9. [CrossRef]
[Pubmed]

21.
Villanova M, Malandrini A, Toti PE, et al. Localization of merosin in the normal human brain: Implications for congenital muscular dystrophy with merosin deficiency. J Submicrosc Cytol Pathol 1996;28(1):1–4.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Arthur Semedo Insumbo - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Zakia El Yousfi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Siham El Haddad - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Latifa Chat - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nazit Allali - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Arthur Semedo Insumbo et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.